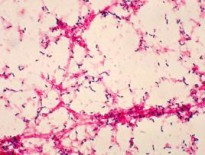
Credit: Blue0ctane / Wikipedia / public domain
When I meet a new patient, I’m frequently astounded by the healthcare he has received. I’ve met patients with absolutely no cardiac symptoms who have been receiving EKGs every six months for years. I’ve had patients brag to me about their annual executive physicals in which myriad tests including treadmill stress tests and chest X rays were routinely performed. Patients get head-to-toe CT scans under the mistaken hope that they might save their lives by finding something. I’ve seen patients with no family history of colon cancers have colonoscopies every two years, because they really want to make sure that they don’t get colon cancer. Some patients do the best they can to be tested for everything.
In the absence of appropriate indications, all these tests are not only without value, they can be harmful. Even in perfectly healthy patients they can yield abnormal results simply through error. (These results are called false positives.) These results then have to be pursued with more invasive tests that can have complications and risks. This isn’t just a theoretical risk. I’ve seen patients harmed by tests that should never have been done.
Doctors are quick (and correct) to roll their eyes when patients take various unproven alternative medicines. When they take Echinacea for their colds, pop their multivitamins, and take black cohosh for menopausal symptoms. Patients should know that what they’re doing is unproven. But it occurs to me that doctors are much less critical when unproven or ineffective interventions are pushed by our colleagues. An unindicated stress test is every bit as unlikely to help a patient as a multivitamin, but potentially riskier. After all, a false positive result from a stress test may lead to an unnecessary angiogram, a risk that the multivitamin doesn’t carry.
The incentives that perpetuate the first type of ineffective medicine – the herbs, supplements, and vitamins – are obvious. Suppliers want to sell their product. They label and advertise their product with messages that fall just below the threshold for fraud, and patients interpret these messages to mean far more than they do. Eager to find something effective for what is frequently an untreatable problem (like a cold) patients understandably flock to these ineffective remedies.
But ironically, ineffective tests and remedies prescribed by physicians have even more perverse incentives. At least the patient has to pay for her own Echinacea and her own vitamins. The pointless EKG and stress test are covered by insurance! In a system in which tests are covered and the prices are fixed by the insurance company, the incentive is to deliver as many tests as possible. The doctor doesn’t lose anything if some of those tests lead to needless anxiety and further invasive testing. The patient doesn’t think to ask questions about the proven risks and benefits because he’s not getting the bill. The incentives do not reward achieving health, or preventing disease, or maximizing patient satisfaction. They reward delivering services. And we’re surprised that the result is the delivery of lots of services with no value.
Escaping the insurance system makes it easier to see the problem more objectively. I get paid by patients to listen to them and give them advice. I don’t get paid more if I order a test, and I also don’t get paid less. And I’m not paid by anyone but the patient. So I can actually take the time to educate the patient about the risks and benefits and figure out if she really wants the test. The net result is that patients pay me more so I can make sure they get more education and less healthcare.
I’ve written before about how our current healthcare market broke and how I believe it could be fixed. I think insurance coverage of routine care is a major flaw in the current system. We are currently expending enormous resources trying to insure everyone. If, as I believe, insurance is the problem and not the solution, the results will be even worse than the broken system we started with.